Abstract

Introduction:
While thrombocytopenia is common and affects 29% of patients (pts) with MDS, severe thrombocytopenia (platelets (plt) <20x109/L) affects approximately 10% of pts and is associated with bleeding and higher risk IPSS-R scores.
Prophylactic and therapeutic plt transfusions are commonly administered to prevent bleeding in pts with MDS and severe thrombocytopenia but are inconvenient and associated with risks. Since the inception of the MDS registry in 2006 at our centre, we commonly administer tranexamic acid (TXA, 1-1.5 grams PO BID-TID) to thrombocytopenic pts with MDS to decrease minor mucosal bleeding and the use of plt transfusions for non-severe bleeds. The administration of prophylactic and/or therapeutic plt transfusions is at the discretion of the treating haematologist.
Objective:
To retrospectively audit the bleeding rates and transfusion requirements of pts with MDS and durable severe thrombocytopenia as related to TXA use, plt transfusions, and disease characteristics.
Methods:
All pts with MDS with durable severe thrombocytopenia (plt count <20x109/L in ≥50% of days over an 8-week period) treated at Sunnybrook Health Sciences Centre and registered in the prospective MDS registry were eligible. Bleeding events, rated with the World Health Organization bleeding scale were captured by registry and chart review. The highest grade bleed experienced by the patient was assigned once for each clinic visit documenting a bleeding event. Platelet transfusion frequency and quantity during the period of severe thrombocytopenia were obtained. Platelet transfusions were considered prophylactic (PROPH) if they occurred at a recurring time interval of ≤2 weeks, and were considered therapeutic otherwise. Descriptive statistics are reported, and ANOVA or correlation coefficients were calculated where relevant.
Results:
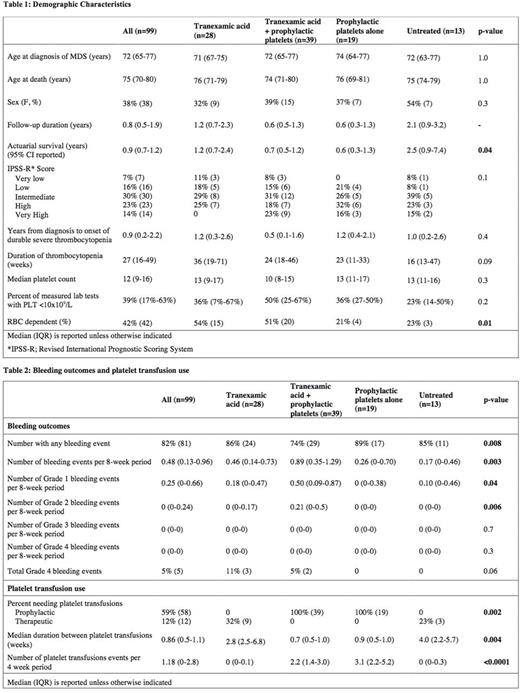
Of 200 pts with severe thrombocytopenia at any time, 99 had durable severe thrombocytopenia and were included. Demographics are presented in Table 1. The pts were classified as receiving TXA alone (n=28), TXA + PROPH, (n=39), PROPH plts alone (n=19) and untreated (n=13). Median time from diagnosis to start of durable severe thrombocytopenia was 0.9 years (IQR 0.2-2.2), duration was 27 weeks (IQR 16-49), and median plt count was 12x109/L (IQR 9-16). Pts receiving TXA +/- PROPH plts had significantly higher rates of concurrent red blood cell transfusion dependence. With a median follow-up of 0.8 years (95% CI 0.6-1.2), actuarial survival was 0.9 years (95% CI 0.7-1.2).
68% of pts were prescribed TXA at any point with a median time from onset of severe thrombocytopenia of 5 weeks (IQR 0-13) and a median duration of 23 weeks (IQR 12-41). Only 32% and 23% of TXA alone and untreated pts respectively required therapeutic plt transfusions at any point with a median time between transfusions of 2.8 and 4.0 weeks respectively. The median number of plt transfusion events per 4-week period was 0 for TXA alone and untreated pts compared with 2.2 and 3.1 events for TXA + PROPH or PROPH alone (p<0.0001) (Table 2).
During the period of severe thrombocytopenia, 82% (81/99) of pts had at least one bleeding event, and 5% (5/99) had a grade 4 bleeding event. There was a significant difference in grade 1 and 2 bleeding rates between groups, with the highest rates in pts on TXA +/- PROPH plts (Table 2). There was no significant difference in grade 3 or 4 bleeding rates between groups.
Conclusions:
Patients with MDS and durable severe thrombocytopenia at a Canadian tertiary care centre had low rates of major bleeding (5%) compared to what has been previously reported in the literature, but poor overall survival. Seventy-one percent of severely thrombocytopenic pts on TXA or no therapy required no therapeutic platelet transfusions for the duration of study follow-up. The benefit of TXA and/or prophylactic platelet transfusions for the prevention of bleeding would be best evaluated in the context of a randomized controlled trial.
Wells: Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees; Alexion: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees. Lin: Pfizer: Honoraria; Pfizer: Other: advisory board; CSL Behring, Grifols: Other: unrestricted education grant; Novartis: Research Funding. Buckstein: Celgene: Honoraria, Research Funding; Astex: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal